About the Retiree Drug Subsidy Program
In 2003, the Medicare Modernization Act (MMA) was signed into law by President George W. Bush. This law created Medicare Part D, which created three distinct Medicare prescription drug plans.
- Employer Group Waiver Plans (EGWP)
- Prescription Drug Plans (PDP)
- Medicare Advantage Prescription Drug Plans (MA-PD)
However, in order to incentivize employers to continue to cover prescription drug costs for their Medicare eligible retirees, the MMA created the Retiree Drug Subsidy (RDS) program which helps to subsidize the financial obligation of Plan Sponsors’. The RDS program is run by the Center for Medicare and Medicaid Services (CMS) under the direction of the Department of Health and Human Services of the Federal Government operating with a RDS payment budget of roughly $6 billion annually.
Under the RDS program, the CMS reimburses Plan Sponsors the equivalent of 28% of all allowable Retiree Drug expenses that fall between the federally designated Cost Threshold amount and the Cost Limit after Actual Cost Adjustments are removed. This amount is limited per individual, which, like the cost threshold and cost limit, varies from year to year. To see this years cost thresholds and limits, click here.
For example, for plan years ending in 2019, the cost threshold is $415 and the cost limit is $8,500.
If an individual had $10,000 in allowable retiree drug expense in 2019…
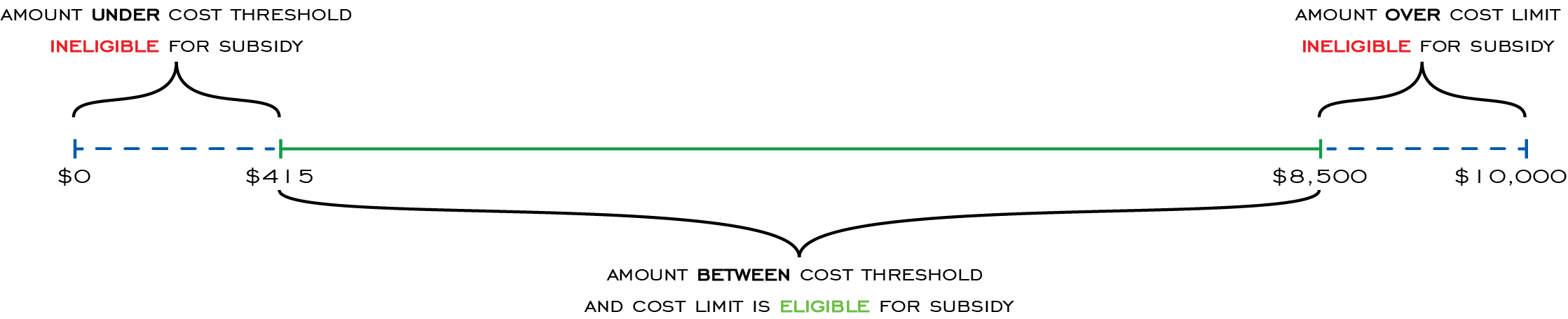
This means that $8,085 of the Retiree’s allowable drug expenses is eligible for the subsidy. At a 28% reimbursement rate, the Plan Sponsor is potentially eligible to collect $2,263.80 in RDS funds for each eligible member.
In order to be eligible to receive this subsidy, individuals and their respective Plan Sponsors must meet certain requirements:
- The individual must be eligible and/or enrolled in Medicare Part A and/or Part B OR have end stage renal disease or other approved disability status.
- Prescription drugs must be Part D eligible.
- The individual must be retired from the Plan Sponsor’s company.
- The Plan Sponsor’s health benefits must be actuarially equivalent to that of Medicare as attested to by an approved actuary.
- Retain application data (actuarial attestation, member claims data, policies and procedures related to cost reporting and data analysis, etc.) in case of CMS Audit.
The RDS Reopening Process
Beginning in 2009, the CMS began allowing both current and former RDS participating Plan Sponsors to reopen their previously reconciled retiree drug subsidy applications to identify missed subsidy and ensure program compliance. In order to reopen RDS applications, Plan Sponsors must apply within four years of the date of the original final reconciliation and they must provide the RDS appeals center with documented “good cause” as to why the reopening should be granted.
Recently, the RDS announced that reopening appeals must now be completed and submitted on the RDS secure site. If the reopening is granted, the Plan Sponsor is then allowed to “redo” the 12 step final reconciliation process on the RDS site starting with Step 2: Review Payment Setup.
12 Step Reconciliation Process
- Initiate Reconciliation
- Review Payment Setup
- Request List of Covered Retirees
- Finalize Covered Retirees Request Reports
- Start Preparation of Reconciliation Payment
- Manage Submission of Final Cost Reports
- Review Final Costs Information
- Enter Revisions to Final Costs
- Finalize Reconciliation Payment Request Information
- Review Electronic Funds Transfer (EFT) Information
- Approve Electronic Funds Transfer (EFT) Information
- Review and Submit Reconciliation Payment Request
Redoing the final reconciliation process allows Plan Sponsors to add new and/or updated information for members such as updated eligibility periods, submit additional Part D eligible drug claims and make other updates or changes to their application to collect previously unidentified subsidy dollars or correct compliance issues.
Helpful Resources
This is the RDS program website that Plan Sponsors use to participate in program. On this site Plan Sponsors create or renew their ongoing retiree drug subsidy applications, confirm which individuals covered by their group health plan are eligible for the RDS program, submit their regular (monthly, quarterly, etc.) subsidy payment requests and complete final reconciliation fifteen months after the plan year ends among many other important program requirements. As a client of Part D Advisors, all of these responsibilities and more are handled for you. All you have to do is sit back and watch the retiree drug subsidy dollars roll in.
The Retiree Drug Subsidy program Welcome Kit website contains everything a new Account Managers, Authorized Representatives, Actuaries, Designees, Vendors or anyone else involved in the RDS program administration of a group health plan could need to know. It breaks down the RDS program into six areas to help simplify the process for Plan Sponsors and offers quick start guides for each user role.
The RDS resource library is a collection of important links and user guides to provide information to new and experienced users alike. It also contains the reconciliation toolkit to help Plan Sponsors complete the 12 step reconciliation process, technical guides for setting up mainframe cost reporting and eligibility queries and web-based training courses to assist users assigned to specific RDS roles.
The Centers for Medicare and Medicaid Services (CMS) is the area of the of Health and Human Services (HHS) department that is responsible for administering the Retiree Drug Subsidy program. On this site you can find more information about the Retiree Drug Subsidy program, as well as many other insurance options and other services provided by the CMS.
