Comprehensive Ongoing RDS Services.
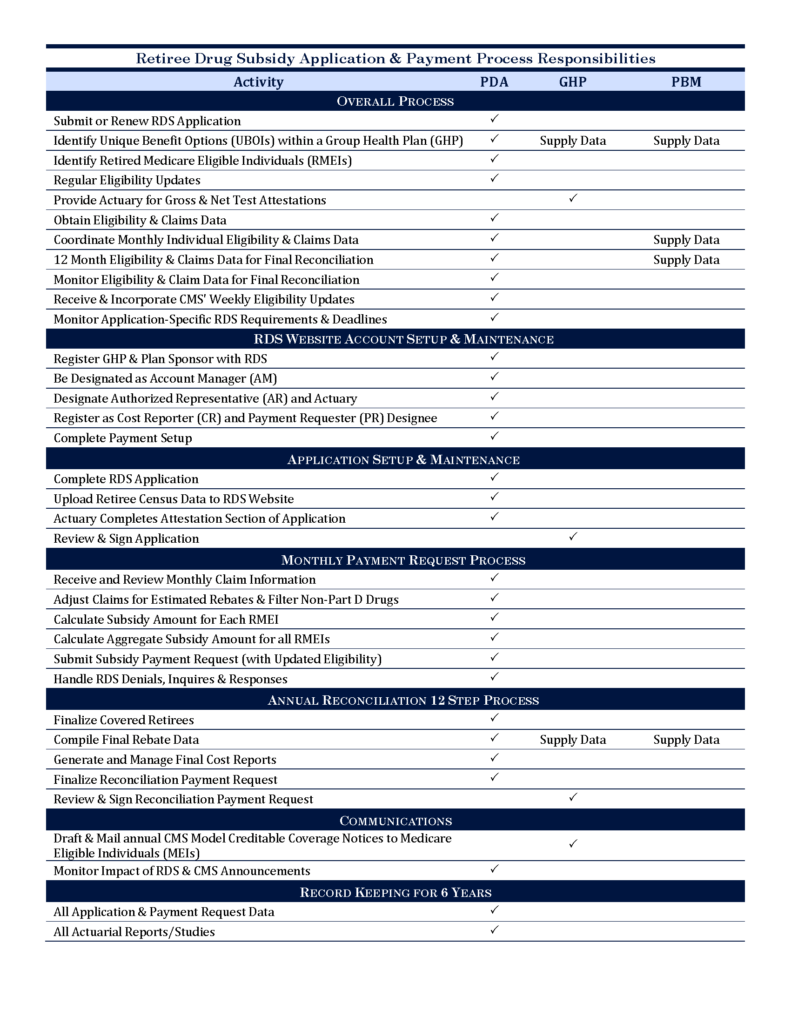
PDA offers our clients the most extensive and effective ongoing RDS services available in the RDS administration marketplace. We handle every possible aspect of the program for Plan Sponsors, including, but not limited to, setting up new applications, managing and regular updates to eligibility records, aggregating monthly data and filing cost reports, compiling rebate data, completing reconciliations, and warehousing all data for the six year term required by the Centers for Medicare and Medicaid Services (CMS).
Our approach allows the Plan Sponsor to remain in the driver’s seat of the RDS process without the hassle of the day to day activities, saving their staff time and money. Additionally, our solution is extremely customizable and allows us to provide a variety of reporting and communication options to keep you updated on all changes and current work projects.
PDA’s clients benefit from our one of a kind claim data processing and from our expert eligibility management system, proprietary drug filtering software and one-of-a-kind new member identification algorithm, which allows Plan Sponsors to maximize their subsidy dollars from every aspect of the RDS program. A full list of our ongoing RDS services can be found below.